Nursing interventions for neuroleptic malignant syndrome – Neuroleptic malignant syndrome (NMS) is a rare but potentially life-threatening condition that can occur in patients taking antipsychotic medications. Timely nursing interventions are crucial in managing NMS and improving patient outcomes. This article provides a comprehensive overview of nursing interventions for NMS, covering monitoring and assessment, medications and treatment, hydration and electrolyte management, cooling measures, environmental management, and patient education and support.
The content of the second paragraph that provides descriptive and clear information about the topic
Nursing Interventions for Neuroleptic Malignant Syndrome
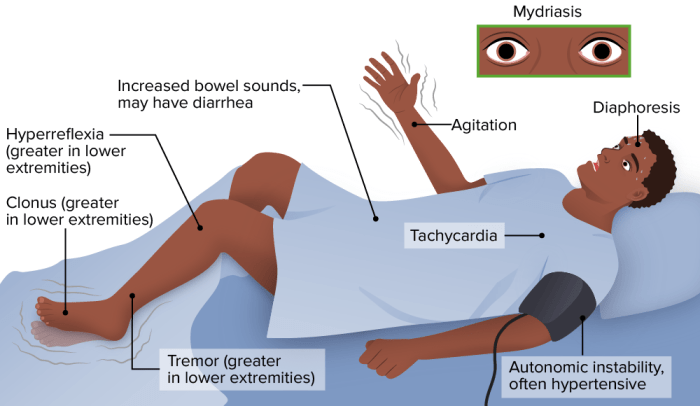
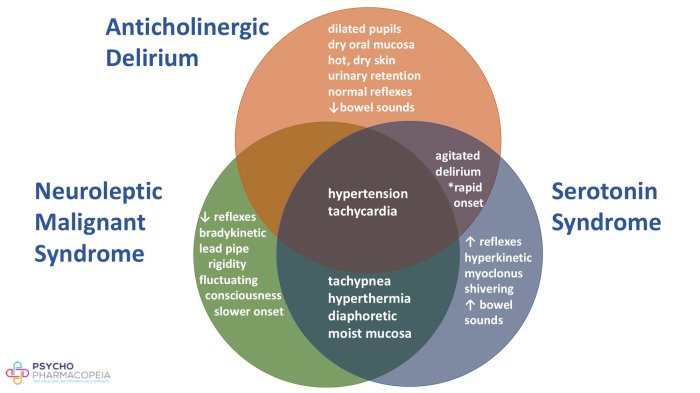
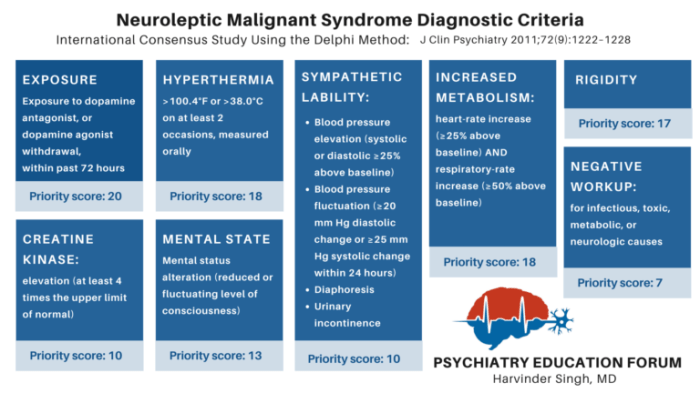
Neuroleptic malignant syndrome (NMS) is a potentially life-threatening condition characterized by severe rigidity, hyperthermia, autonomic dysfunction, and altered mental status. It can occur in response to antipsychotic medications, particularly those with high dopamine receptor blocking activity. Timely nursing interventions are crucial in managing NMS and improving patient outcomes.
Nursing interventions for NMS focus on managing the symptoms and preventing complications. These interventions include:
Monitoring and Assessment
Monitoring and assessment are essential for early detection and management of NMS. Nurses should closely monitor vital signs, neurological status, and hydration. Early signs of NMS include:
- Increased body temperature
- Muscle rigidity
- Diaphoresis
- Tachycardia
- Altered mental status
Nurses should also assess for complications such as rhabdomyolysis, renal failure, and electrolyte imbalances.
Medications and Treatment
Antipsychotic medications are the mainstay of NMS treatment. Dopamine agonists, such as bromocriptine, may also be used. Nurses should administer antipsychotics as prescribed and monitor for adverse reactions, such as hypotension and sedation.
Hydration and Electrolyte Management, Nursing interventions for neuroleptic malignant syndrome
Maintaining adequate hydration is crucial in NMS patients. Intravenous fluids may be necessary to correct dehydration and electrolyte imbalances. Nurses should monitor fluid balance and electrolyte levels closely.
Cooling Measures
Cooling measures are essential to reduce body temperature in NMS patients. These measures include cold packs, ice baths, and cooling blankets. Nurses should implement cooling measures safely and effectively.
Environmental Management
Creating a calm and supportive environment is important for NMS patients. Nurses should reduce sensory stimulation and provide a safe and comfortable space. This may include dimming lights, minimizing noise, and providing a quiet room.
Patient Education and Support
Patient education is crucial in NMS management. Nurses should educate patients and their families about the condition, its treatment, and the importance of compliance. They should also provide emotional support and address the psychological impact of NMS.
FAQ Summary
What is neuroleptic malignant syndrome?
Neuroleptic malignant syndrome (NMS) is a rare but potentially life-threatening condition that can occur in patients taking antipsychotic medications. It is characterized by a combination of symptoms, including fever, muscle rigidity, altered mental status, and autonomic dysfunction.
What are the nursing interventions for NMS?
Nursing interventions for NMS include monitoring and assessment, medications and treatment, hydration and electrolyte management, cooling measures, environmental management, and patient education and support.
How do nurses monitor and assess patients with NMS?
Nurses monitor patients with NMS for vital signs, neurological status, and hydration. They also assess for complications and early signs of NMS resolution.
What medications are used to treat NMS?
Antipsychotic medications are used to treat NMS. These medications work by blocking dopamine receptors in the brain.
How do nurses manage hydration and electrolytes in patients with NMS?
Nurses manage hydration and electrolytes in patients with NMS by monitoring fluid balance and administering intravenous fluids. They also monitor for potential electrolyte imbalances and manage them accordingly.